Does Ice Help in the Healing Process?
Understanding the Historical Context of Ice in Injury Management
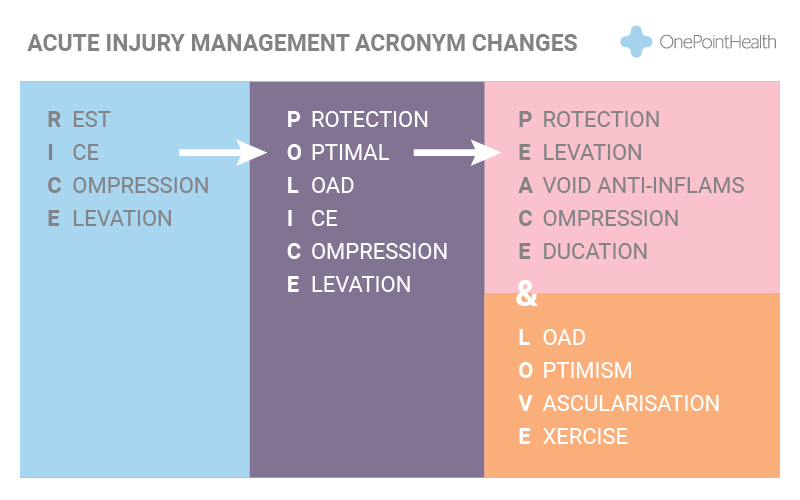
The discussion surrounding the use of ice in sports medicine and acute injury rehab has evolved significantly over the years. The concept of using ice, initially popularised in the RICE protocol (Rest, Ice, Compression, Elevation), has been deeply ingrained in our culture since 1978. The intention behind incorporating ice was to minimise the inflammatory response and thereby accelerate healing.
Revisiting the Science Behind Ice and Inflammation
However, the evolution of research has led to a reconsideration of the role of ice in injury management. The shift from RICE to POLICE (Protection, Optimal Loading, Ice, Compression, Elevation) in 1992 highlighted the importance of optimal loading for recovery, acknowledging that rest or a lack of movement could be detrimental.
Analgesic Properties of Ice: A Double-Edged Sword?
The efficacy of ice as an analgesic (pain-numbing agent) is well-established in the literature. It effectively cools the skin’s temperature, providing short-term relief. Yet, the impact on underlying muscles is questionable, as muscle temperature remains largely unchanged with topical ice application. The key question emerges: does ice contribute to the healing process in the mid to long-term?
The Shift in Expert Opinion: Dr. Gabe Mirkin’s Retraction
In 2014, Dr. Gabe Mirkin, the originator of the RICE protocol, acknowledged changes in research findings and retracted ice from his initial recommendations. He pointed out that both ice and complete rest might delay healing instead of facilitating it. The crucial aspect he referred to is the body’s natural inflammatory response, where signals prompt the release of Insulin-like Growth Factor (IGF-1) to initiate healing. Applying ice may impede this natural release, potentially hindering the healing process.
Introducing a New Protocol: PEACE & LOVE
The paradigm shift in 2019 resulted in the emergence of a new protocol: PEACE & LOVE (Protection, Elevation, Avoid Anti-Inflammatory Drugs, Compression, Education & Load, Optimism, Vascularisation, and Exercise). This comprehensive approach emphasises factors beyond simply minimising inflammation and recognises the importance of various elements in the recovery process.
Evaluating the Pros and Cons of Ice in Modern Rehabilitation
The newfound evidence against the use of ice prompts a critical question: if ice delays healing, even if it provides temporary pain relief, should it still be a standard practice? The answer, according to the presented information, leans towards a negative stance. The acknowledgment of the benefits of the inflammation process and the potential hindrance caused by ice raises concerns about its overall efficacy in injury management.
However, there’s a crucial caveat – in cases where excessive swelling poses a threat to recovery, such as severe joint sprains or situations with significant oedema, ice may still be a viable option. The goal shifts from preventing all swelling to limiting its extent. In instances where muscle tears result in less oedema, the efficacy of ice in early injury management becomes questionable.
Rethinking the Routine Application of Ice
In conclusion, based on the current research, the general recommendation is to reconsider the routine use of ice. While acknowledging that some inflammation is part of the recovery process, the emphasis shifts towards encouraging safe return to movement as soon as practical. Ice, it seems, is less important than once thought, with exceptions for cases where swelling is a limiting factor for recovery.
The evolving landscape of sports medicine prompts a nuanced approach, recognising the complexities of individual injuries and tailoring interventions accordingly.